How to Interpret Hemolysis Labs Results
Hemolysis is the breakdown of red blood cells (RBCs), which release hemoglobin into the bloodstream. This process can occur naturally in the body as part of RBC turnover, but it can also be induced by certain conditions, diseases, or laboratory procedures. Hemolysis can significantly affect the accuracy and interpretation of various laboratory tests, particularly in blood samples. Therefore, understanding how to interpret hemolysis lab results is essential for healthcare providers to make accurate diagnoses and avoid misinterpretation of results.
What is Hemolysis?
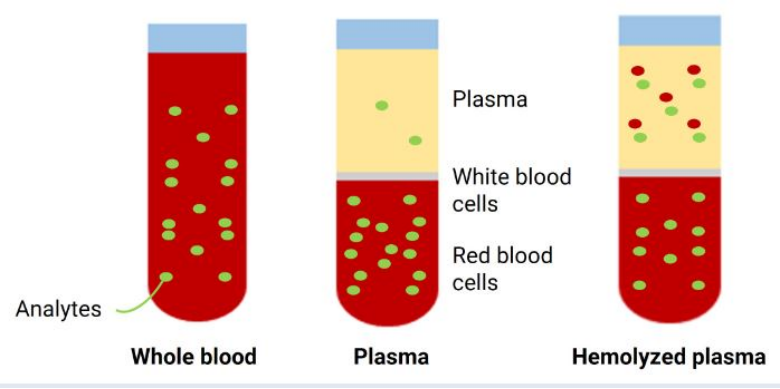
Hemolysis refers to the rupture of RBCs, leading to the release of hemoglobin and other intracellular components into the plasma. This process may occur in two forms: in vivo (within the body) or in vitro (during laboratory sample collection, handling, or processing). In vivo hemolysis can be a sign of various medical conditions, such as hemolytic anemia, infections, or autoimmune disorders. On the other hand, in vitro hemolysis typically results from factors such as improper collection techniques, rough handling, or prolonged storage of the blood sample.
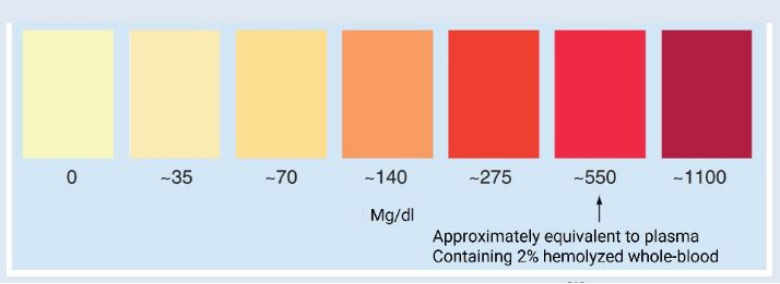
How to Recognize Hemolysis in Lab Results
Laboratories commonly perform visual assessments to detect hemolysis in blood samples. Hemolysis can cause the plasma or serum to turn pink, red, or even brownish, depending on the extent of RBC destruction. This is often referred to as "hemolyzed" plasma. The presence of hemolysis can lead to inaccuracies in lab tests, particularly those measuring analytes found in the RBCs (e.g., potassium, lactate dehydrogenase, and hemoglobin).
Laboratory Tests Affected by Hemolysis
Several laboratory tests can be significantly impacted by hemolysis, potentially leading to incorrect diagnoses or the need for retesting. Some tests that are sensitive to hemolysis include:
● Potassium: Hemolysis releases potassium from RBCs, leading to falsely elevated potassium levels in the plasma. This can mimic hyperkalemia, which can be a life-threatening condition if not properly evaluated.
● Lactate Dehydrogenase (LDH): LDH is abundant in RBCs, and hemolysis can cause artificially high LDH levels. High LDH can also indicate tissue damage, so the source of the elevation must be carefully interpreted.
● Hemoglobin: Elevated levels of hemoglobin in plasma due to hemolysis can lead to misinterpretation in tests that measure hemoglobin, such as hematocrit.
● Bilirubin: As RBCs break down, bilirubin is released. Hemolysis can lead to an artificially high serum bilirubin level, which can be mistaken for liver disease.
Evaluating Hemolysis Lab Results
When interpreting hemolysis in lab results, it’s crucial to consider the extent of the hemolysis and the potential impact on test outcomes. If hemolysis is suspected in a sample, it is essential to:
Examine the Sample: Visual inspection is the first step. Blood that appears pink or red may indicate hemolysis.
Review Patient History: If hemolysis is detected, consider the patient's clinical presentation. If the hemolysis is in vivo, it could be a sign of an underlying condition like hemolytic anemia or an infection.
Check Test Results: Some tests, such as potassium, LDH, and hemoglobin, can be skewed by hemolysis. Compare the results with the clinical picture and consider repeating the test with a new sample if necessary.
Consider Retesting: If hemolysis is suspected to have impacted the results, a new blood sample should be collected and handled carefully to prevent further hemolysis.
Preventing Hemolysis in the Lab
Preventing hemolysis is crucial to ensuring accurate test results. Some key preventive measures include:
● Using the correct needle size to minimize trauma during blood collection.
● Avoiding excessive force when drawing blood and ensuring smooth handling of the sample.
● Storing blood samples at the proper temperature and avoiding prolonged storage.
● Gently mix the blood sample to prevent clotting or hemolysis.
Conclusion
Hemolysis can significantly impact the accuracy of laboratory test results. By understanding how to recognize, interpret, and address hemolysis labs results, healthcare providers can avoid misdiagnoses and ensure more accurate clinical decision-making. Whether caused by medical conditions or improper sample handling, recognizing hemolysis and taking appropriate action is essential for optimal patient care.








2748